Key Takeaways
- GLP-1 medications have multiple side effects, all of which are important to know when considering whether or not to use one to assist in your weight loss journey. One side effect can be the creation of loose skin, which may necessitate plastic surgery after significant weight loss.
- GLP-1 medications themselves don’t directly cause loose skin. But because they can lead to rapid and significant weight loss, the skin may not have time—or elasticity—to shrink back. The result is sagging folds, most often on the abdomen, arms, thighs, and sometimes the chest.
- For people struggling with hygiene, mobility, or confidence due to extra skin, surgical removal (such as panniculectomy (apron removal, or excess skin removal from the lower abdomen), tummy tuck, or arm/thigh lifts can be an option once weight has stabilized.
Losing weight—especially with the help of GLP-1 medications like semaglutide (Ozempic®, Wegovy®) or liraglutide (Saxenda®)—is an accomplishment worth celebrating. Many patients lose 15–20% of their body weightin clinical trials. As the study’s publication points out:
“The coprimary end points were the percentage change in body weight from baseline to week 72 and a weight reduction of 5% or more at week 72. Key secondary end points included weight reduction of 10% or more, 15% or more, and 20% or more at week 72; the change in weight from baseline to week 20; and the change from baseline to week 72 in waist circumference, systolic blood pressure, fasting insulin and lipid levels, and the physical function score on the 36-Item Short Form Health Survey (SF-36), version 2, acute form. The percentage change in total body-fat mass from baseline to week 72 was assessed in a subgroup of 255 participants who underwent dual-energy x-ray absorptiometry.” (Wilding et al., NEJM 2021; Jastreboff et al., NEJM 2022)
This is a significant, life-changing transformation that has potential for improving blood sugar levels, heart health, and overall energy. (Wilding JPH, et al., 2023)
But along with those victories comes a new and often frustrating challenge: excess amounts of loose skin. Long-term weight changes can gradually reduce the skin’s ability to tighten on its own (Sami et al., 2015; Gallo et al., 2019; Hany et al., 2024; Wilding et al., 2021; Jastreboff et al.,2022).
“The etiology of skin laxity after rapid weight loss is inadequately understood. It usually occurs because of damage of collagen and elastin, which allows for no skin retraction after weight loss.
Macromolecular components of connective tissue are dependent on age, gender, nutritional imbalances, hormones, including those of pregnancy, use of certain drugs and chemicals, and assorted genetic and environmental factors, including prolonged exposure to sunlight and other forms of radiating energy.” (Sami, et al, 2015)
In this article, we provide an overview of GLP-1 medications, the effects of rapid weight loss, and for whom plastic surgery for excess skin removal is a good option. We know that your weight loss journey is highly personal, and any step to a healthy and more active lifestyle is something to be celebrated. That’s why it’s important to understand the benefits and risks of GLP-1 medications, and how secondary side effects such as excess skin may factor into your overall experience.
What Are GLP-1 Medications?
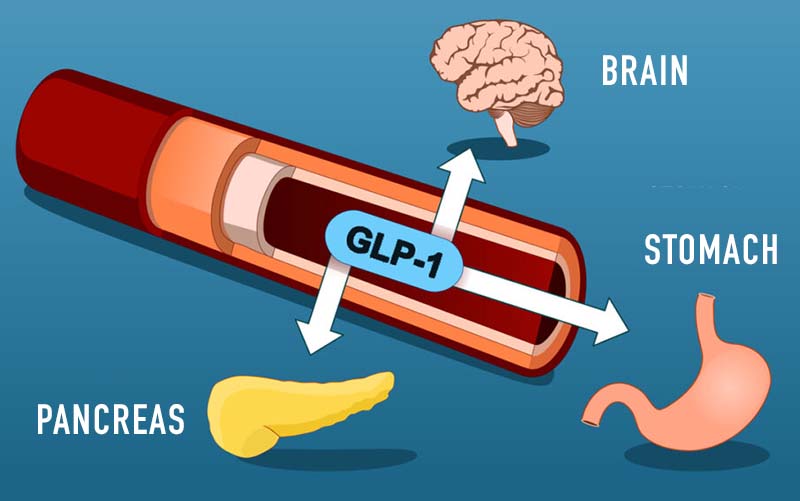
GLP-1 (glucagon-like peptide-1) receptor agonists are prescription drugs that mimic the natural hormone GLP-1. They:
- Signal fullness to your brain, helping reduce appetite
- Slow digestion, so you feel satisfied longer
- Improve blood sugar by boosting insulin release
Common GLP-1 medications:
 There are several GLP-1 medications on the market, going by different names
There are several GLP-1 medications on the market, going by different names
- Semaglutide (Ozempic®, Wegovy®)
- Liraglutide (Saxenda®)
- Tirzepatide (Mounjaro®, Zepbound® — a dual GIP/GLP-1 agonist)
These medications are FDA-approved for type 2 diabetes management and, at higher doses, for chronic weight management. They work in slightly different ways and can lead to different amounts of weight loss. The table below provides a clear, side-by-side comparison of their dosing, approved uses, and average results in clinical studies.
| Medication | Brand Names | How It’s Taken | FDA-Approved Uses | Average Weight Loss in Studies | Key Notes |
| Semaglutide | Ozempic® (diabetes), Wegovy® (weight loss) | Weekly injection | Type 2 diabetes, chronic weight management | ~15% of body weight (NEJM 2021) | Very effective; once-weekly dosing is convenient |
| Liraglutide | Saxenda® (weight loss), Victoza® (diabetes) | Daily injection | Type 2 diabetes, chronic weight management | ~8% of body weight (NEJM 2015) | Older option; works but requires daily shots |
| Tirzepatide | Mounjaro® (diabetes), Zepbound® (weight loss) | Weekly injection | Type 2 diabetes, chronic weight management | Up to ~20% of body weight (NEJM 2022) | Newest option; works on GLP-1 + GIP pathways, highest average weight loss so far |
GLP-1 Weight Loss Efficacy Studies and Research
How much weight a person loses varies between individuals; different factors that affect results include genetics and lifestyle. However, there are multiple studies behind these drugs highlighting certain results, including these two of note:
- In one major trial, semaglutide users lost an average of 15% body weight (Wilding et al., 2021).
- Tirzepatide showed losses up to 20% in another study (Jastreboff et al., 2022).
GLP-1 Primary Side Effects
Like all medications, GLP-1 receptor agonists can cause side effects. The most common ones are related to the digestive system, while a few more serious effects are rare but important to be aware of.
Most common (GI-related):
- Nausea and vomiting – especially when first starting or increasing the dose
- Diarrhea or constipation – changes in bowel habits are frequent
- Abdominal discomfort or bloating – due to slower stomach emptying
(Wilding et al., NEJM 2021; Jastreboff et al., NEJM 2022)
Less common but reported:
- Headache and fatigue – usually mild and temporary
- Injection site reactions – redness, itching, or swelling
Rare but important:
-
- Gallbladder disease (including gallstones and cholecystitis) – a 2022 meta-analysis found increased risk, especially at higher doses and longer use (He et al., JAMA Intern Med 2022, PMC8961394)
- Pancreatitis (inflammation of the pancreas) – rare, but potentially serious; seek medical attention if you have severe abdominal pain
- Kidney problems from dehydration – usually related to vomiting or diarrhea if fluids aren’t replaced
GLP-1 Secondary Side Effects
In addition to the well-documented gastrointestinal and metabolic effects, some patients also experience changes in body appearance as a result of weight loss itself. These are not direct drug side effects, but rather a consequence of how quickly and how much weight is lost while on therapy.
Secondary side effects of GLP-1 medications may include:
- Loose or sagging skin: especially around the abdomen, arms, thighs, and chest
- Changes in body contour: areas that once carried more fat may look deflated
- Skin irritation under folds: moisture and friction can lead to rashes or infections
- Psychological impact: frustration or disappointment when excess skin hides weight-loss progress
Clinical studies confirm that rapid, high-percentage weight loss—like the 15–20% averages seen with semaglutide and tirzepatide—makes patients more likely to experience loose skin (Wilding et al., NEJM 2021; Jastreboff et al., NEJM 2022).
While not medically dangerous in itself, excess skin can cause real problems: discomfort, hygiene issues, and emotional distress. This is where skin-removal surgery becomes part of the conversation—not as a cosmetic luxury, but often as a functional and quality-of-life treatment.
Why Does Rapid Weight Loss Cause Excess Skin?
Skin is elastic, but only up to a point. Over time at a higher weight, the skin’s natural support structures (collagen and elastin) can lose some of their resilience. After rapid weight loss, the skin may not always contract fully to your new shape (Sami et al., Plast Surg Int 2015).
Key Factors Affecting Excess Skin After Weight Loss
- Amount and speed of weight loss
- Age: Age can influence skin elasticity, with skin generally becoming less flexible over time.
- Genetics: Individual differences in skin elasticity are strongly influenced by genetic factors.
- Lifestyle: Smoking, sun exposure, and poor protein intake can damage collagen over time.
The GLP-1 Clinical Connection
While GLP-1 medications support meaningful weight loss and health benefits, the speed and degree of that loss may contribute to the development of loose skin.
Managing Excess Skin After GLP-1 Weight Loss
Non-surgical Excess Skin Treatment Options
Not all loose skin requires surgery. Some patients find improvement with:
- Strength training: Building muscle mass can help fill out and firm areas of mild laxity.
- Balanced nutrition: Adequate protein, hydration, and micronutrients support skin health.
- Skin-tightening devices: Radiofrequency, ultrasound, or laser-based treatments can offer modest tightening for mild sagging.
These approaches are most effective when skin looseness is mild to moderate. For more significant folds, however, surgical removal is typically the only reliable option.
When to Consider Skin-Removal Surgery After Rapid Weight Loss
If you’ve reached your weight-loss goals with a GLP-1 medication but are left struggling with excess skin, you may be wondering whether plastic surgery is the right solution for you. While every medical procedure has its own risks, plastic surgery for excess skin is an option for those who are a good candidate. Surgeons look at several factors to make that determination. Our board-certified plastic surgeon, Dr. Nick Masri, uses the following criteria to determine whether his patients are able to safely go through this procedure.
Who Is a Good Candidate for Skin-Removal Surgery After GLP-1 Weight Loss?
A good candidate for skin removal surgery after GLP-1 weight loss typically displays:
Consistent Weight
Keeping your weight within a steady range for three to six months is often a sign you may be ready for skin-removal surgery. Surgeons don’t require you to reach a “perfect” number on the scale — the focus is on stability, body contour, and your overall health. In fact, many patients continue to lose additional weight after surgery as their metabolism adjusts during recovery.
Overall Good Health
Conditions like uncontrolled diabetes, heart disease, or smoking can make surgery riskier. Optimizing your health first creates a safer environment for healing.
Realistic Expectations
Skin-removal surgery reshapes the body and relieves discomfort from folds, but it also leaves scars. Knowing both the benefits and limitations helps you feel confident in your decision.
A note for patients with high Body Mass Index (BMI): You do not need to be at a “normal” BMI. Many patients remain in the overweight or obese range and still qualify. The surgeon will individualize your plan based on safety, goals, and skin concerns.
Common Procedures for Excess Skin Removal after Taking a GLP-1 Medication
Excess skin can appear in more than one area, and there isn’t a single procedure that works for everyone. A reputable surgeon will recommend the appropriate procedure for your unique needs and goals for removing excess skin. Different procedures target specific areas. More specifically:
Panniculectomy (or lower abdomen skin removal):
Removes a large overhanging “apron” of skin from the lower abdomen. May be considered medically necessary (and potentially covered by certain insurance plans) if it causes rashes, infections, or hygiene problems.
Abdominoplasty (tummy tuck)
Abdominoplasties tighten abdominal skin and muscles for contour. Usually considered cosmetic.
Brachioplasty (arm lift):
Brachioplasties remove loose skin, including that caused by GLP-1 weight loss, from the upper arms.
Thigh lift:
Reshapes thighs by removing inner- and outer-thigh folds.
Breast lift/augmentation (mastopexy ± implants):
Sometimes, it is considered after massive weight loss if the chest has significant sagging or volume loss.
Your surgeon may recommend staging procedures over time for safety and optimal results.
Benefits and Risks of Skin-Removal Surgery
Every surgery comes with advantages and potential drawbacks. Understanding both sides can help you make a well-informed, confident decision with your surgical team.
Benefits
For many people, skin-removal surgery provides not only physical relief but also meaningful improvements in daily life. The benefits extend beyond appearance, helping with comfort, mobility, and overall well-being.
Relief from rashes and skin infections
Removing folds of excess skin can reduce areas where moisture and friction collect, lowering the risk of chronic irritation or infections.
Easier mobility and exercise
Excess skin can make movement uncomfortable. Surgery often restores freedom of motion, making daily activities and physical exercise more enjoyable.
Better hygiene
By removing skin that traps sweat and bacteria, many patients find it easier to stay clean and comfortable throughout the day.
Improved self-confidence and comfort in clothing
Beyond physical relief, surgery can make clothing fit better and help patients feel more at ease in social and personal settings.
Risks
While skin-removal surgery can bring many benefits, it’s important to remember that every operation carries potential risks. Most complications are uncommon and can often be managed effectively, especially when surgery is performed by a board-certified plastic surgeon and you follow recovery instructions closely. Knowing these possibilities upfront helps you make an informed, confident decision.
Risk of infection or delayed healing
Like any operation, there is a chance of wound infection or slower-than-expected recovery. Following aftercare instructions closely reduces this risk.
Risk of bleeding or blood clots
Complications such as bleeding or clot formation are uncommon but possible. Surgeons take steps to prevent these issues with careful planning and monitoring.
Permanent but visible scars
All skin-removal procedures leave scars. Most fade over time, but it’s important to be prepared for lasting marks.
Possibility of revision surgery
In some cases, additional procedures may be needed to refine results or address healing concerns.
The Patient Journey of Surgery for Excess Skin Removal after Taking GLP-1
At our Miami plastic surgery practice, most patients considering skin-removal surgery have either used or are currently using GLP-1 medications. For many, these drugs were a boost after weight-loss surgery or when other methods stalled. In some cases, Dr. Masri recommends GLP-1 therapy to help patients reach a safer weight for surgery. Their stories are remarkably similar — GLP-1s help them move forward, and surgery provides the final step in achieving comfort and contour.
Consultation: Beginning the Conversation
Medical review and history
Your surgeon will carefully review your health background, including your GLP-1 use, overall medical conditions, and lifestyle. This ensures your plan is safe and tailored to you.
Physical exam and photographs
Expect a respectful, detailed exam to assess where excess skin is most problematic. Photos may be taken to help plan your surgery and track your progress.
Discussion of goals and risks
This is your chance to talk openly about what bothers you most, what you hope to achieve, and what outcomes are realistic. Your surgeon will also explain the benefits and potential risks so you can make an informed choice together.
Preparation: Setting Yourself Up for Success
Stabilizing your weight
Maintaining your new weight for 6–12 months reassures your surgeon that your results will last and your body is ready for surgery.
Optimizing nutrition
A balanced diet rich in protein, vitamins, and hydration supports healing and recovery. Think of it as fueling your body for the final (and ongoing) stages of your journey.
Lifestyle adjustments
Quitting smoking, controlling blood sugar, and managing other health conditions greatly reduce surgical risks and improve healing.
Medication guidance
Some anesthesiologists may recommend stopping GLP-1 medications 2–3 weeks before elective surgery, in line with current guidance from the American Society of Anesthesiologists (ASA, 2023). This precaution helps reduce the risk of gastroparesis (slowed stomach emptying) and aspiration during anesthesia, especially in higher-risk patients.
However, updated multisociety guidance released in 2024 (ASA, AGA, ASMBS, ISPCOP, SAGES) notes that many patients can continue their GLP-1 medications safely before surgery. The decision is ultimately made case by case by the anesthesia team, considering your health, comorbidities, and procedure type.
Surgery Day
Every practice is different, and at our plastic surgery practice in Miami, we take extra care to ensure your comfort and peace of mind. These procedures are always performed in one of the accredited Memorial Hospitals in Miami. We recommend never trading a hospital for a plastic surgery clinic, even if a clinic offers lower prices.
Anesthesia and comfort
Skin-removal procedures are done under general anesthesia, so you’ll be asleep and pain-free.
Post Procedure: In or Outpatient
Many patients go home the same day, while more extensive surgeries may involve an overnight stay for monitoring and comfort.
Recovery: Healing and Adjusting
Immediate aftercare
Compression garments, wound care, and gentle walking are part of the early recovery process. These steps support healing and reduce complications.
Gradual return to activity
Over weeks to months, you’ll slowly increase movement. Your surgeon will guide you on when it’s safe to resume lifting, exercise, and daily routines.
Scar care
Scars are a natural part of healing. With time, care, and sun protection, they typically fade, leaving you with smoother contours and improved comfort.
Long-Term Care: Maintaining Your Excess Skin Removal Surgery Results
Weight stability
Keeping your weight steady helps preserve your surgical results. Large fluctuations can stretch the skin again.
Ongoing support
Regular follow-ups with your surgical team ensure your scars are healing, your results are lasting, and your emotional well-being is supported.
Confidence in your new chapter
For many patients, this phase marks a turning point — the chance to fully enjoy the health gains from GLP-1 therapy without the physical and emotional burden of excess skin.
FAQs
How long after GLP-1 weight loss can I have surgery?
Most surgeons recommend waiting until your weight has been stable for 3-6 months.
Will insurance cover skin-removal surgery?
Panniculectomy may be covered if strict criteria are met (rashes, infections, pannus below the pubic area). Abdominoplasty and most lifts are considered cosmetic, and therefore not covered by insurance.
Is surgery safe for high-BMI patients?
Yes — with the right precautions, many patients with higher BMI can safely undergo skin-removal surgery. What matters most is risk stratification, not just the number on the scale. For example, a healthy 24-year-old with obesity may have a very different risk profile than a 45-year-old with a normal BMI but a history of smoking or recent steroid use. Experienced surgeons take all of these factors into account, using careful staging and safety protocols. Our double board-certified head plastic surgeon, Dr. Nick Masri, has guided thousands of patients through body-contouring procedures after GLP-1 weight loss, tailoring each plan to the individual’s health and goals.
How painful is recovery?
Recovery related pain will depend on a variety of factors, including which procedure a patient is undergoing, and your surgeon should be able to walk you through expectations specific to you as well as options for pain management. Speaking in general terms, you can expect soreness for 1–2 weeks, managed with pain control and support garments. Most people resume normal activities within 2 weeks, depending on the procedure.
In Conclusion: Is Plastic Surgery After Rapid GLP-1 Weight Loss The Best Option For You?
If excess skin is limiting your comfort or confidence after GLP-1 weight loss, you’re not alone. Every person’s situation is different, and if non-surgical skin tightening options aren’t delivering the results you need, plastic surgery may be a suitable option depending on your overall health and other factors.
The best way to know is to schedule a consultation with a board-certified plastic surgeon to discuss whether skin-removal surgery is right for you. Every journey is unique, and compassionate care can help you feel at home in your body again.
READY TO DISCUSS YOUR OPTIONS WITH DR. NICK?
About Dr. Nidal Masri
 Dr. Nidal “Nick” Masri is a double board-certified plastic surgeon with over 25 years of experience. What sets him apart is his expertise in body contouring for high BMI and post-bariatric patients, an area where many surgeons lack the specialized knowledge needed for optimal results. Known for his straightforward, safety-first approach, Dr. Masri has become one of Florida’s most trusted names in post-weight loss plastic surgery.
Dr. Nidal “Nick” Masri is a double board-certified plastic surgeon with over 25 years of experience. What sets him apart is his expertise in body contouring for high BMI and post-bariatric patients, an area where many surgeons lack the specialized knowledge needed for optimal results. Known for his straightforward, safety-first approach, Dr. Masri has become one of Florida’s most trusted names in post-weight loss plastic surgery.
Disclaimer
This educational content does not replace personalized medical advice. Always consult a qualified clinician about your specific situation.
References
- Wilding JPH, Batterham RL, Calanna S, et al. (2021). Once-Weekly Semaglutide in Adults with Overweight or Obesity. New England Journal of Medicine, 384(11), 989–1002. doi:10.1056/NEJMoa2032183.
- Jastreboff AM, Aronne LJ, Ahmad NN, et al. (2022). Tirzepatide Once Weekly for the Treatment of Obesity. New England Journal of Medicine, 387(3), 205–216. doi:10.1056/NEJMoa2206038.
- Pi-Sunyer X, Astrup A, Fujioka K, et al. (2015). A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. New England Journal of Medicine, 373(1), 11–22. doi:10.1056/NEJMoa1411892.
- He L, Wang H, Guo Y, et al. (2022). Association of GLP-1 Receptor Agonist Use With Risk of Gallbladder and Biliary Diseases: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Internal Medicine, 182(5), 513–519. PMC8961394. doi:10.1001/jamainternmed.2022.0339.
- Wilding JPH, et al. (2023). Semaglutide and Cardiovascular Outcomes in Patients with Overweight or Obesity (SELECT Trial). New England Journal of Medicine, 389(22), 2059–2070. doi:10.1056/NEJMoa2307563.
- Sami K, El Khatib A, Shady I, et al. (2015). Image Analyzer Study of Skin in Morbid Obesity and After Massive Weight Loss. Plastic Surgery International, 2015, 1–9. PMC4311578. doi:10.1155/2015/303647.
- Gallo JRB, Santos J, Oliveira F, et al. (2019). Skin Protein Profile after Major Weight Loss: Collagen and Elastic Fiber Analysis. International Journal of Molecular Sciences, 20(18), 4637. PMC6756662. doi:10.3390/ijms20184637.
- Hany M, Farag M, El-Sheikh M, et al. (2024). Histological Skin Changes After Massive Weight Loss. Aesthetic Plastic Surgery, 48, 123–132. PMC10899414. doi:10.1007/s00266-023-03247-0.
- Boswell CB, Symbas JD, Nahai F, et al. (2010). Body Contouring Following Massive Weight Loss. Seminars in Plastic Surgery, 24(3), 219–226. PMC6188338. doi:10.1055/s-0030-1262974.
- Langer V. (2011). Body Contouring Following Massive Weight Loss. Indian Journal of Plastic Surgery, 44(2), 246–253. PMC3111107. doi:10.4103/0970-0358.85342.
- Cadwell JB, Fligor SC, Sheth N, et al. (2021). Panniculectomy Outcomes by Body Mass Index: Analysis of 12,732 Cases. Obesity Surgery, 31(8), 3660–3666. PMC8187133. doi:10.1007/s11695-021-05461-0.
- Stumpfe MC, Dietz A, Seitz T, et al. (2024). Laboratory Markers in Body Contouring after Bariatric Interventions. Clinical, Cosmetic and Investigational Dermatology, 17, 45–53. PMC11210174. doi:10.2147/CCID.S392153.
- Dalaei F, Heden P, Hansson E, et al. (2024). Body Contouring After Bariatric Surgery Improves Long-Term Health-Related Quality of Life. Annals of Surgery, 279(6), 1125–1134. PMC11086676. doi:10.1097/SLA.0000000000006008.
- American Society of Plastic Surgeons (ASPS). (2019). Insurance Coverage Criteria for Panniculectomy. Policy Paper. Available at: https://www.plasticsurgery.org.
- Anthem, Inc. (2025). CG-SURG-99 Panniculectomy and Abdominoplasty (Medical Policy). Available at: https://www.anthem.com.
- American Society of Anesthesiologists (ASA). (2023). Consensus-Based Guidance on Preoperative Management of Patients on GLP-1 Receptor Agonists. ASA News Release, June 29, 2023. Available at:https://www.asahq.org/about-asa/newsroom/news-releases/2023/06/american-society-of-anesthesiologists-consensus-based-guidance-on-preoperative
- ASA, AGA, ASMBS, ISPCOP, SAGES. (2024). Most Patients Can Continue GLP-1 Receptor Agonists Before Elective Surgery and Endoscopy: Multisociety Clinical Practice Guidance. October 29, 2024. Available at:https://www.asahq.org/about-asa/newsroom/news-releases/2024/10/new-multi-society-glp-1-guidance
- U.S. Food and Drug Administration (FDA). (2025). FDA Launches Green List to Protect Americans from Illegal Imported GLP-1 Drug Ingredients. FDA Press Announcement, July 2025. Available at:https://www.fda.gov/news-events/press-announcements/fda-launches-green-list-protect-americans-illegal-imported-glp-1-drug-ingredients
